Improving healthcare access
Reducing the barriers to receiving good care, closer to home.


Across our region, more people can access the right care when they need it. Through partnerships with general practice, allied health providers, community organisations and hospital networks, we've worked to make primary health care more accessible, inclusive and responsive.
Through our combined efforts, we're helping people connect to safe, inclusive care in their local community.
Scroll to explore ↓
What we've achieved

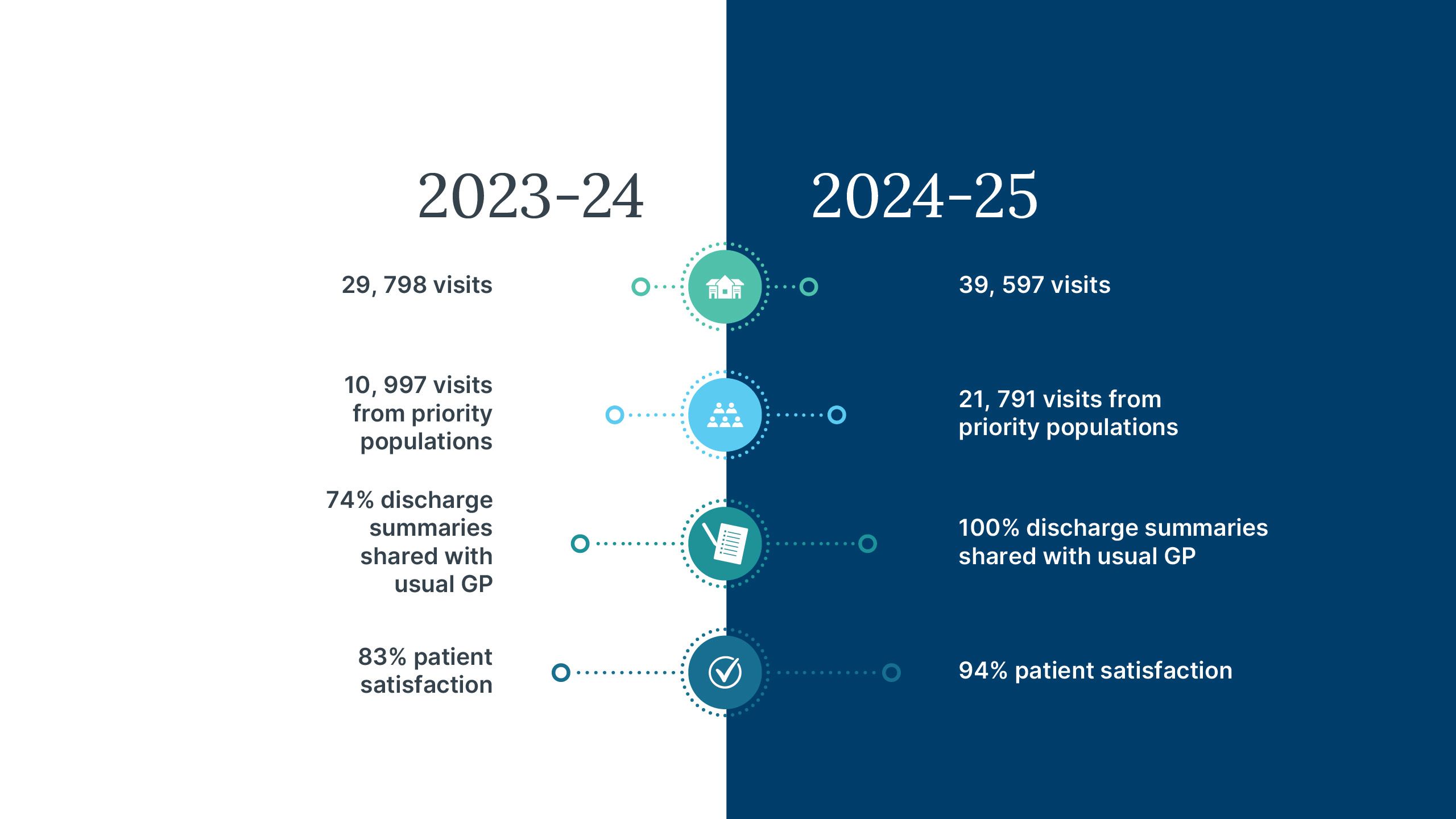
Medicare Urgent Care Clinics: Doubled access, increased care coordination
The Medicare Urgent Care Clinic program has continued to grow, marked by the commissioning of the Oxley Urgent Care Clinic in December 2024, joining the Logan (Browns Plains) and South Brisbane clinics.
Collectively, the 3 Medicare Urgent Care Clinics doubled service delivery this year, providing bulk-billed, accessible urgent care that helps people avoid long waits in hospital emergency departments for non-life-threatening health conditions.
This year, Medicare Urgent Care Clinics delivered:
- 39,597 episodes of urgent care (doubled from 19,790 last year)
- 21,791 episodes of care to people from priority population groups* (nearly doubled from 10,997 recorded last year)
- 100% of discharge summaries shared with usual GP* (compared to 74% last year)
- 94% patient satisfaction rate (improved from 83% last year)
*Nearly half of all episodes of care (45%) were provided to patients with culturally and linguistically diverse backgrounds, First Nations peoples, older persons, people with disability and non-Medicare eligible patients. This demonstrates the clinics are reaching people who often face barriers accessing timely care.

Medicare Urgent Care program expansion announced
From December 2025 to February 2026, an additional 3 Medicare Urgent Care Clinics are opening in Carindale, Capalaba and Holland Park–Yeronga, moving our region closer to the national target of 4 in 5 Australians living within 20 minutes of a Medicare Urgent Care Clinic.
“When patients need urgent care for conditions, such as a twisted ankle, minor burns and infections, cuts requiring suturing—Medicare Urgent Care Clinics offer a bulk-billed alternative to visiting a hospital emergency department if they can’t see their usual GP for same-day treatment.”
Image caption: Medicare Mental Health Center Redlands.
Image caption: Medicare Mental Health Center Redlands.
Redland Medicare Mental Health Centre
Redland Medicare Mental Health Centre
Medicare Mental Health Centres: Free, walk-in support when people need it
We opened 2 Medicare Mental Health Centres in Logan (November 2024) and Redlands (December 2024), removing cost and wait-time barriers that can prevent people from seeking mental health support in the moments it is needed. The walk-in model of care provides direct connection to supports, proving transformative for people who otherwise may have been discouraged from seeking mental health help.
Since opening, the Medicare Mental Health Centres have:
- received more than 2,300 referrals for service
- recorded more than 3,500 service contacts
- operated at full capacity, demonstrating substantial previously unmet need.
Service features have been co-designed with local communities for safety and inclusion:
- Peer workers in teams reduce stigma and create welcoming environments. Someone who’s lived through mental health challenges greeting people as they arrive fundamentally changes the tone and reduces fear.
- First Nations community engagement roles ensure cultural safety for Aboriginal and Torres Strait Islander people who may have experienced discrimination or cultural unsafety in mainstream mental health services.
- Connection to ongoing support rather than just crisis intervention—centres help people establish sustainable mental health care pathways, not just respond to immediate crises.
Care when it's needed: One person's story of access to free, walk-in mental health care during their ‘windows of readiness’
One Logan centre guest experiencing homelessness, substance use challenges and mental health crisis arrived with high distress and suicidal ideation. Over 4 months of walk-in support—attending when they felt able, without rigid appointment schedules—they:
- secured a Mental Health Care Plan
- connected with an ongoing psychologist
- achieved stable employment
- found stable housing.
This reflects what becomes possible when access barriers are removed. Walk-in availability meant this person could access support during their ‘windows of readiness’, rather than being turned away because they didn't have an appointment or couldn't afford the fees.

Open Doors: Providing safe spaces for LGBTIQA+SB young people
We co-funded Open Doors Youth Service to open a hub in Logan—Queensland's only youth service specifically for LGBTIQA+SB (lesbian, gay, bisexual, transgender, intersex, queer, asexual, Sistergirl and Brotherboy) young people. The opening was a response to health data insights and direct feedback from young people who had voiced that they didn't always feel safe accessing mainstream mental health services.
Since the Logan opening in March 2025, Open Doors has supported 175 young people in 6 months, providing a safe, affirming environment where identity is understood and respected, not met with scepticism or dismissed.
Services include case management, counselling, peer groups and family sessions—addressing mental health, housing, substance use, family relationships and identity support in integrated ways.
A young person's story of finding inclusive support through Open Doors to re-engage with life pathways
A young person with a disability who had been removed from their family home and was experiencing school disengagement and uncertainty about their identity after recently coming out as gay, worked with Open Doors for 5 months and:
- successfully re-engaged with school
- developed peer connections with other LGBTIQA+SB young people
- returned to a safe home environment with improved family relationships
- increased their NDIS funding to better support their disability needs
- improved their self-advocacy skills
- is now preparing for employment with ongoing Open Doors support.
Creating safe, affirming spaces where LGBTIQA+SB young people can access mental health care addresses a critical equity gap. Rapid uptake—175 young people in just 6 months—demonstrates how significant the need and gap in inclusive care was felt within current mainstream services.

Refugee Occupational Therapy: Removing barriers to NDIS access
Many people from refugee and asylum-seeker backgrounds need functional capacity assessments for NDIS access or disability supports, but assessments cost around $2,000—far beyond reach for newly arrived families on income support. This left GPs unable to connect patients to the support they clearly needed.
We funded the Mater Refugee and Asylum Seeker Occupational Therapy Program to become the first free functional-assessment service in our region.
In just 7 months of operation there were:
- over 250 interventions addressing functional impairment and fall risk
- 46 Medical Aid Subsidy Scheme applications securing wheelchairs, walkers, shower chairs, hospital beds
- 10 NDIS Functional Capacity Assessments enabling access to NDIS supports
- 7 home modifications assessed and implemented
- 27 general practices referring patients.
Over 90% of clients assessed were at risk of falls. One in 5 were at risk of hospitalisation without timely intervention. Early occupational therapy intervention prevented adverse outcomes such as falls leading to fractures, hospitalisations, loss of independence.

Village Connect: Cultural connection and community building enables access to healthcare
In connection with our Pasifika and Māori Health and Wellbeing Strategy, Brisbane South PHN funded programs delivered through Village Connect that supported more than 1,600 Pasifika and Māori families this year—that’s 9 times higher than past reported healthcare engagement rates for Pasifika and Māori peoples with mainstream services.
The exceptional engagement in programs reflects what can be achieved when programs are co-designed with the communities they serve, delivered in familiar community settings, and led by people who share cultural context.
Through this support, families were connected to:
- culturally safe GP services for better chronic disease management and preventive care
- social supports (housing, income support, family services, legal assistance)
- intergenerational wellbeing programs
- maternal health support through Pasifika Maternity Hub
- mental health support through Side-by-Side project
- health system navigation assistance provided in familiar language and settings.
Feature story: Elders nurture culture and friendships that strengthened individual wellbeing

Learn more about how Brisbane South PHN is improving health outcomes for people and communities in our region.






